I wanted to share this article, by a co-worker writing anonymously. It really resonated with me, thinking back to my parents’ problems adapting to the ever-evolving digital tools that swept mechanical devices aside. It feels to me that the marketing need for change is in direct conflict with the familiarity our elders depend on, especially those with memory problems. – Ray Shah, founder, Think Design
Reading time: 11 min
![]()
The monkeys are in the telephone exchange
My mother has mild dementia. She knows who she is and who I am. She knows who many other people are and what to do at what time of day; if she knows what time of day it is. She’s quite present in the moment but anything that requires memory of more than language, or linear and not momentary experience, is difficult.
For example, we may have a good chat about my day and her day and whatever comes to mind, and then, if there’s a moment’s silence, we may have it again. The facts she states might align with what others will also say happened or they may be conflated with some other day or time—we all do this, of course, but not with such incontinence of the mind.
She may look at something she’ll recognize and comment on it, look away, and in looking back see it for the first time. So, every email is a new email, no matter how it tries to show it has been read; each letter a new letter, no matter if it’s no longer in an envelope. What’s in a drawer is not what’s expected, if anything is expected. In this respect, she believes everything in her apartment is being moved by others and she can’t find anything. Object recognition is patchy. Phones and TV remotes are interchangeable. Spoken words are usually the right words, but sometimes the monkeys are in the telephone exchange.
Being lost in familiar places happens occasionally, but she has good homing instincts, not yet disappearing for very long. Still, she has recently become frightened when losing her sense of place, shaking her confidence for a while.
Blaming dementia
Amid this, she has a strong sense of rightness. Things that go wrong are not going wrong because of her.
And of course, she is right. Given her capacity, she is not capable of doing anything wrong. But if we want to lay blame—and doesn’t the world love blame—then dementia is the culprit.
Mum’s fiercely independent spirit—having lived alone for more than 20 years, having cared for everyone else, having handled everything thrown at her—now creates a sense of victimization; of things being done to her and around her without her consent. No matter how careful anyone is to involve her, she cannot remember it. Even kindness, feeling imposed, becomes a tyranny. This aspect of dementia is a deep and cruel well.
Physically, she’s in good shape for her age, though historic issues create present problems. She’s unsteady, walking with the aid of a stick, or being wheeled in a wheelchair if out and needing to go more than a few dozen steps.
Mostly, her loss of independence has been mitigated by professional carers, by the visits of friends and neighbors who care, and by us, her children and grandchildren taking up regular tasks. I live abroad and my sister lives nearby. My sister, therefore, bears the brunt of care outside that which other carers can provide. It’s brought burnout. The person Mum was is not the person she is. For some, that provokes resentment.
Still, in good moments, on good days, for Mum there is no problem. Certainly, we and she are fortunate to be in the position to afford care. Many are not and can’t cope at all.
How simple to summarize all the emotional trauma and disconnection that dementia brings into a few matter-of-fact paragraphs. The human aspect will always go beyond retelling, beyond measurement. What Mum feels, she feels as deeply as she ever did.
50 million people out of their mind
Dementia comes to many, perhaps 50 million people have it today. It comes in many forms, being itself a syndrome, a catchall that encompasses several usually progressive disorders causing chronic memory loss, personality changes or impaired reasoning. Often, those faculties’ diminishment is intertwined. The word itself—from the Latin demens, dement, meaning “out of one’s mind”—is imbued with negativity and fear.
There is a huge effort to address dementia across the world, especially as the world’s population ages and the proportion of the aged increases. It will be one of the biggest social challenges of the coming century.
I work in social tech, at the intersection of homelessness and technology, believing that technology should be built for the public good. It can and does help as much as it hinders. It could help much more. As Mum changes, I have been wondering what technology could do for people with dementia, puzzling over it as any layperson might.
Can technology overcome dementia?
I write here having explored and considered what I’ve seen, hopefully just a fraction of what there is. I won’t critique any particular project or product since I have no first-hand experience of their use, but I will say that much of what I’ve seen relies on some remnant of linear thinking and the ability to learn new habits. It all looks crazily complicated for where Mum is at and must be aimed at earlier or milder forms of dementia.
Framing Mum’s relationship with tech; she was born in the early 1930s and has lived in England all her life, so everything we are now familiar with and dependent on through home and mobile technology in the ‘First World’ she first started seeing in her mid-40s. I remember the family TV remote control, the “clicker”—which also meant having a TV on which you could channel the channel with a loud clap—and the strangeness of having an Acorn computer at home. The mobile phone was a few years away when I was trying to learn Basic. Mum used a personal computer for about 30 years, until about a year ago when she just couldn’t figure out how to use it anymore.
When I’m with her, and remotely, I help Mum by going through everything patiently and carefully, knowing that no matter how many times I do it will not stick. She may get things working herself; sometimes she can turn the TV on, and sometimes it will be on the right channel. It may be a struggle to turn off though, so plugs or wires get pulled. Funny how those things stick–to turn something off, to stop it doing what it’s doing, yank at it! Other habitual things may be done perfectly, or at least, well enough. The microwave is impossible, but the oven possible. Reading instructions on the back of a pre-prepared dish and then going to enact them, also impossible. Once she’s looked away from the instruction and looked at the cooking device, she’s forgotten what she read.
I’ve watched this stressful back and forth from the oven to the kitchen counter, as Mum gets more irritable and upset at her incapacity, somehow still realizing the concept of failure, of believing herself to being capable until this moment. “I’ve been doing this perfectly, on my own, all my life,” is her most common refrain. Encouraging Mum to do things without thinking, to just do what feels natural, has had some success. But only if I’m there to remind her.
With such limits, I think about this application of tech in terms of helping Mum maintain a semblance of independence (a codependence), rather than providing a cure.
External memory
Asking what technology can do for people who cannot remember, the answer is…
It depends on the stage of dementia a person is at, for if you have no memory, you cannot function independently.
Memory, in that respect, defines survival for living beings. If there is nothing instinctive or innate, then there is inaction and death. If there is no ability to learn, physically or mentally, then there is no evolution, and that likely means extinction.
For machines, memory defines action. If there is no impulse from memory, there is no on or off; there is nothing. Initially outsourced to their human operator—the “computer”—memory is now built into every device.
Technology can help
The digital products available for people living with dementia appear to fall into 3 broad categories:
- Those that are memory and communication aids, which assist carers as well as the person with dementia
- Those that are alarms and warnings, which are mainly to inform carers of possible danger
- Those that are for involvement, stimulation, or simply to be comforting—basically, adult toys
There are products and practices which address social exclusion or loneliness, and these certainly impact an existential aspect of dementia, but they are not built to help only sufferers of dementia, being designed to enable vital human connection at a variety of ages and life stages. Also, there is robotics, which will in the future produce any number of physical human helpers, whether mimicking the human or animal form or not. Robot helpers look like they will cement codependence—what a marketing opportunity that is! Certainly, if we stay on the current path, robot helpers will become indispensable technology.
My day to day work, with people who are homeless, is rooted in human-centered design, which sees ideas, products, and processes iteratively flow from the needs and behaviors of potential users. This is “building with, not for,” aiming to arrive at what is most useful and helpful through utilizing the expertise of lived experience and marrying it to the creative leap.
I have been interested to see human-centered design applied to some of the more recent digital innovations around solutions for those suffering from dementia, such as those which competed for the Smart Ageing Prize in 2017. It’s great for society to have this practice proliferate into engaging senior citizens. I hope to involve Mum in some design sessions and have signed her up for a particular organization’s outreach. Being valued never loses its appeal!
Software updates break connections
And yet… and yet… technology cannot overcome. Damaging things is par for the course in the growth-obsessed, change-obsessed world we inhabit, and one of the things that get damaged is elderly people.
If you decide to refresh your brand and redesign your icons (let alone interaction and gestures) in a graphical user interface update, then as a consequence you will break the recognition patterns and muscle memory a person with early dementia relies on. And it won’t matter in this case whether they’ve grown up with technology or not. This is going to happen to all of us that look at a phone now and choose apps by the way the icon looks, its position on our screens or how we click and swipe. In our old age, we will be stabbing at icons on our devices randomly if we don’t escape the concept of GUI updates being core to the business plan.

iOS 1 (2007), iOS5 (‘11), iOS10 (‘13) and iOS13 (‘19) home screens (source images: Wikipedia)
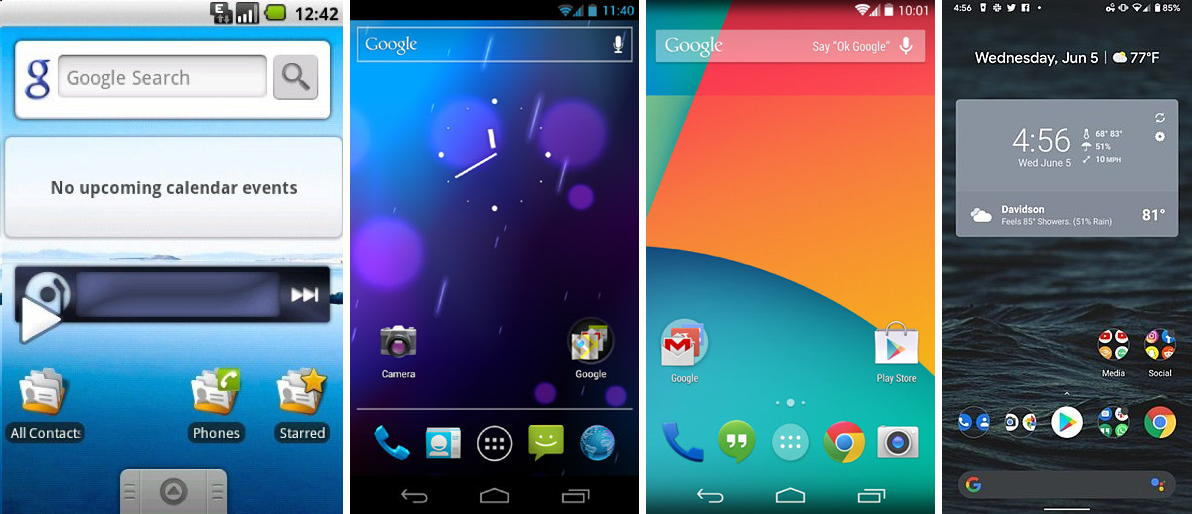
Android Cupcake (2008), Ice Cream Sandwich (‘11), Kitkat (‘13) and Q (‘19) home screens (source images: Wikipedia)
If advances in embeddable technology reach the point where thought control and virtual visualization is possible, we will be thinking about what we want, and it will appear. But most readers of this over fifty won’t have long enough for that world to become habitual. I expect that in their old age, they will experience this as being assailed by their thoughts made real.
Once you cannot learn a new thing, your survival depends on what has been learned. If what has been learned becomes redundant, you are made incapable.
In technology, whenever we break with the past, we put a full stop on someone’s life.
SmartOS
Updates, while they might be carefully constructed to account for learned behaviors, don’t do empathy. Or if they do, I haven’t noticed it yet. We need a truly SmartOS which recognizes where its user’s learning has stopped and maintains the look and feel of previously learned interaction; folding in and hiding every new update behind a small iteration on the already known, aging gracefully by enabling some slow, human-paced and humanly conceivable changes.
Aging in each other’s company allows us to look very different across the years, to become different people and yet stay remembered, trusted. Many aspects combine to maintain continuity, including relatively intangible things like one’s personality. If you walked out of a room and the next minute came back looking like a different person, or suddenly 10 years older, then not even those that know you would think you were still you. Except that your personality might be so similar that, well, OK, maybe it is you, we might believe you based only on our familiarity with your operating system.
Some of us choose to be ‘rebranded’ in the same way updates are pushed, becoming utterly unrecognizable in ways that can fracture relationships. A few people who undergo such extreme change also find they break themselves. As it is now an accepted norm to destroy through reinvention, they are victims of a wider pattern
The best HCD product ever
If future generations grow up with digital tools that have artificial empathy, like the Primers from “The Diamond Age”, or the digital assistant from “Her”, then they may form meaningful and lasting digital connections. Emotional bonds persist into deep dementia.
For now, and for the foreseeable future, it will not happen. We have invented and become economically harnessed to a pace of change that far outstrips natural human capacity.
I love the work companies and individuals are doing to help people with dementia. It has goodness at heart. But the best, most robustly tested human-centered design product we can currently offer our elderly loved ones is not in the realm of technology. It is the family.

